Abnormal development of the pulmonary veins may result in either partial or complete anomalous drainage back into the systemic venous circulation.
TAPVR is a congenital disorder characterized by total mixing of systemic venous blood and pulmonary venous blood within the heart. This complete mixing of venous blood produces cyanosis. In contrast, partial anomalous pulmonary venous return (PAPVR) is usually an acyanotic condition.
The history, physical signs, and electrocardiographic and radiographic findings of PAPVR and TAPVR are similar to those seen in patients with an isolated ostium secundum atrial septal defect (ASD). In some cases, an anomalous vein that drains into the inferior vena cava appears on chest radiography as a crescentic shadow of vascular opacity (like a scimitar) along the right border of the cardiac silhouette (scimitar syndrome). In these patients, an associated ASD is not seen; rather, pulmonary sequestration and anomalous arterial supply to the affected lobe of the lung are encountered.
Preferred examination
For patients with anomalous pulmonary venous return, echocardiography is the preferred examination. The echocardiogram demonstrates an enlarged right ventricle and a small left atrium. It may also show the pattern of abnormal pulmonary venous connections. When the pattern of Doppler venous flow of the abdominal veins is obtained, the finding of venous flow away from the heart is pathognomonic of TAPVR below the diaphragm. Shunting occurs almost exclusively from right to left at the atrial level.
Electrocardiograms demonstrate right ventricular hypertrophy, usually a qR pattern in V3, R, and V1. The P waves are frequently tall and spiked.
TAPVR is a cyanotic lesion. Echocardiographic results usually confirm the diagnosis. MRI and fast CT are also useful for defining pulmonary venous drainage. With cardiac catheterization, the presence of anomalous pulmonary veins may be demonstrated by means of selective pulmonary arteriography.[7, 8]
Sometimes, in anomalous pulmonary venous return, echocardiographic views are limited, and MRI may be necessary.
Radiography
In older children, radiographic findings indicating that the anomalous pulmonary veins enter the innominate vein and that persistent left superior vena cava is present are pathognomonic for anomalous pulmonary venous return. A large supracardiac shadow together with the normal cardiac shadow may have a "snowman" appearance.
Even in patients without obstruction, the heart is enlarged, the pulmonary artery and right ventricle are prominent, and the pulmonary vascularity is increased. In neonates with marked pulmonary venous obstruction, the chest radiograph demonstrates a perihilar pattern of pulmonary edema and a small heart.
In cases of partial anomalous pulmonary venous return (PAPVR) in which more than 2 pulmonary veins have anomalous drainage, right ventricular dilation, pulmonary hypertension, and increased pulmonary blood flow in the lung fields are characteristically seen. Occasionally, the superior vena cava is dilated or an azygous vein or a left vertical vein is present.
The most interesting finding is encountered in cases in which there is anomalous drainage of the right pulmonary veins into the inferior vena cava. In such cases, the pulmonary venous pattern exhibits a crescent-shaped or scimitar-shaped curve along the right heart border in the right lower lung field (scimitar syndrome).
The degree of confidence is moderate. The "snowman" appearance is not helpful for diagnosis in early infancy because of the thymus. False-positive and false-negative results are rare. In patients with pulmonary obstruction, findings of pulmonary congestion and a small heart may be misinterpreted as indicating primary pulmonary disease.
CT-SCAN
Fast CT is useful for defining pulmonary drainage. The degree of confidence is good for anomalous pulmonary venous return. False-positive and false-negative results are rare in anomalous pulmonary venous return.
MRI is useful for defining pulmonary venous drainage. On MRI, anomalous pulmonary venous return is evidenced by a lack of pulmonary veins to the left atrium; the presence of anomalously routed pulmonary veins; a large right atrium; a large right ventricle; a right-to-left interatrial shunt; and, possibly, asymmetry of the pulmonary vasculature. Gradient-refocused gradient echo imaging (eg, FIESTA) in a short-axis stack covering the entire atria is particularly helpful for identifying pulmonary venous return. Two-dimensional cine phase contrast is particularly helpful for identifying and quantifying shunt flow.[9, 10]
Total Anomalous Pulmonary Venous Return
TAPVR and PAPVR
Must have ASD for survival
All have anatomical L to R shunt at atrial level
All have functional R to L shunt of oxygenated blood to right side of heart
--Two Types
lPartial (PAPVR)
-Mild physiologic abnormality
- Usually asymptomatic
Total (TAPVR)
l Serious physiologic abnormalities
Partial Anomalous Pulmonary Venous Drainage (PAPVR)
General
- One of the four pulmonary veins may drain into right atrium
-Mild or no physiologic consequence
-Associated with ASD
-Sinus venosus or ostium secundum types
Total Anomalous Pulmonary Venous Drainage (TAPVR)
-All have shunt through lungs to R side of heart
-All must also have R to L shunt for survival
-Obligatory ASD to return blood to the systemic side
-All are cyanotic
-Identical oxygenation in all four chambers
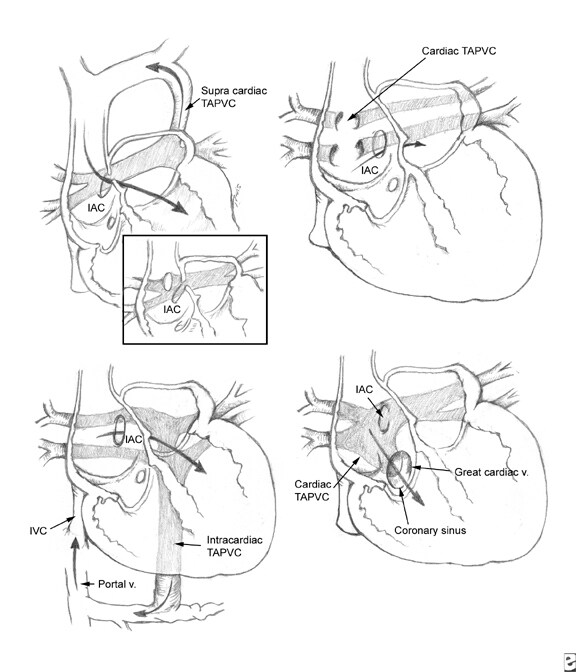
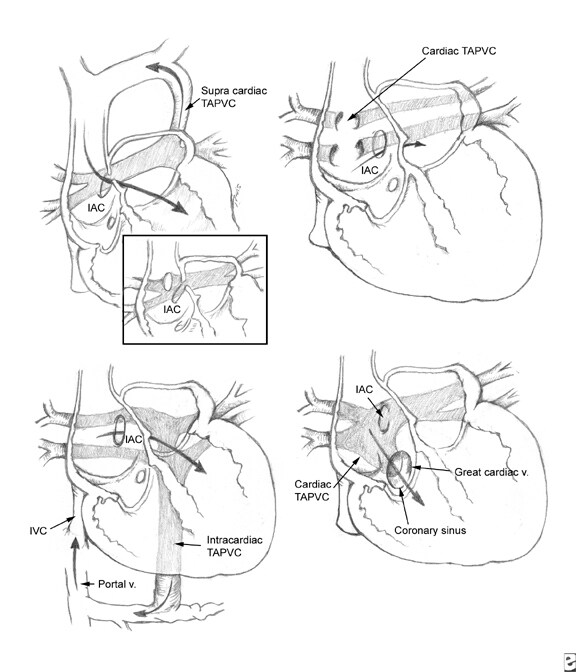
Types
-Supracardiac
-Cardiac
-Infracardiac
-Mixed
Supracardiac Type—Type I
- Most common (52%)
- Pulmonary veins drain into vertical vein (behind left pulmonary artery) to left brachiocephalic vein to SVC
l DDx: VSD with large thymus
Supracardiac Type 1—X-ray Findings
l Snowman heart = dilated SVC+ left vertical vein
l Shunt vasculature 2° increased return to right heart
l Enlargement of right heart 2° volume overload
Cardiac Type—Type II
l Second most common: 30%
l Drains into coronary sinus or RA
l Coronary sinus more common
l Increased pulmonary vasculature
l Overload of RV leads to CHF after birth
l 20% of I’s and II’s survive to adulthood
l Remainder expire in first year
Infracardiac Type—Type III
l Percent of total: 12%
l Long pulmonary veins course down along esophagus
l Empty into IVC or portal vein (more common)
l Vein constricted by diaphragm as it passes through esophageal hiatus
l Severe CHF (90%) 2° obstruction to venous return
l Cyanotic 2° right to left shunt through ASD
l Associated with asplenia (80%), or polysplenia
l Prognosis = death within a few days
Mixed Type—Type IV
l Percent of total: 6%
l Mixtures of types I – III
Three major clinical patterns of total anomalous pulmonary venous return (TAPVR) are seen:
- Severe pulmonary venous obstruction
- Early heart failure
- Mildly symptomatic or asymptomatic TAPVR.
TAPVR is a congenital disorder characterized by total mixing of systemic venous blood and pulmonary venous blood within the heart. This complete mixing of venous blood produces cyanosis. In contrast, partial anomalous pulmonary venous return (PAPVR) is usually an acyanotic condition.
The history, physical signs, and electrocardiographic and radiographic findings of PAPVR and TAPVR are similar to those seen in patients with an isolated ostium secundum atrial septal defect (ASD). In some cases, an anomalous vein that drains into the inferior vena cava appears on chest radiography as a crescentic shadow of vascular opacity (like a scimitar) along the right border of the cardiac silhouette (scimitar syndrome). In these patients, an associated ASD is not seen; rather, pulmonary sequestration and anomalous arterial supply to the affected lobe of the lung are encountered.
Preferred examination
For patients with anomalous pulmonary venous return, echocardiography is the preferred examination. The echocardiogram demonstrates an enlarged right ventricle and a small left atrium. It may also show the pattern of abnormal pulmonary venous connections. When the pattern of Doppler venous flow of the abdominal veins is obtained, the finding of venous flow away from the heart is pathognomonic of TAPVR below the diaphragm. Shunting occurs almost exclusively from right to left at the atrial level.
Electrocardiograms demonstrate right ventricular hypertrophy, usually a qR pattern in V3, R, and V1. The P waves are frequently tall and spiked.
TAPVR is a cyanotic lesion. Echocardiographic results usually confirm the diagnosis. MRI and fast CT are also useful for defining pulmonary venous drainage. With cardiac catheterization, the presence of anomalous pulmonary veins may be demonstrated by means of selective pulmonary arteriography.[7, 8]
Sometimes, in anomalous pulmonary venous return, echocardiographic views are limited, and MRI may be necessary.
Radiography
In older children, radiographic findings indicating that the anomalous pulmonary veins enter the innominate vein and that persistent left superior vena cava is present are pathognomonic for anomalous pulmonary venous return. A large supracardiac shadow together with the normal cardiac shadow may have a "snowman" appearance.
Even in patients without obstruction, the heart is enlarged, the pulmonary artery and right ventricle are prominent, and the pulmonary vascularity is increased. In neonates with marked pulmonary venous obstruction, the chest radiograph demonstrates a perihilar pattern of pulmonary edema and a small heart.
In cases of partial anomalous pulmonary venous return (PAPVR) in which more than 2 pulmonary veins have anomalous drainage, right ventricular dilation, pulmonary hypertension, and increased pulmonary blood flow in the lung fields are characteristically seen. Occasionally, the superior vena cava is dilated or an azygous vein or a left vertical vein is present.
The most interesting finding is encountered in cases in which there is anomalous drainage of the right pulmonary veins into the inferior vena cava. In such cases, the pulmonary venous pattern exhibits a crescent-shaped or scimitar-shaped curve along the right heart border in the right lower lung field (scimitar syndrome).
The degree of confidence is moderate. The "snowman" appearance is not helpful for diagnosis in early infancy because of the thymus. False-positive and false-negative results are rare. In patients with pulmonary obstruction, findings of pulmonary congestion and a small heart may be misinterpreted as indicating primary pulmonary disease.
CT-SCAN
Fast CT is useful for defining pulmonary drainage. The degree of confidence is good for anomalous pulmonary venous return. False-positive and false-negative results are rare in anomalous pulmonary venous return.
MRI is useful for defining pulmonary venous drainage. On MRI, anomalous pulmonary venous return is evidenced by a lack of pulmonary veins to the left atrium; the presence of anomalously routed pulmonary veins; a large right atrium; a large right ventricle; a right-to-left interatrial shunt; and, possibly, asymmetry of the pulmonary vasculature. Gradient-refocused gradient echo imaging (eg, FIESTA) in a short-axis stack covering the entire atria is particularly helpful for identifying pulmonary venous return. Two-dimensional cine phase contrast is particularly helpful for identifying and quantifying shunt flow.[9, 10]
Total Anomalous Pulmonary Venous Return
TAPVR and PAPVR
Must have ASD for survival
All have anatomical L to R shunt at atrial level
All have functional R to L shunt of oxygenated blood to right side of heart
--Two Types
lPartial (PAPVR)
-Mild physiologic abnormality
- Usually asymptomatic
Total (TAPVR)
l Serious physiologic abnormalities
Partial Anomalous Pulmonary Venous Drainage (PAPVR)
General
- One of the four pulmonary veins may drain into right atrium
-Mild or no physiologic consequence
-Associated with ASD
-Sinus venosus or ostium secundum types
Total Anomalous Pulmonary Venous Drainage (TAPVR)
-All have shunt through lungs to R side of heart
-All must also have R to L shunt for survival
-Obligatory ASD to return blood to the systemic side
-All are cyanotic
-Identical oxygenation in all four chambers
Types
-Supracardiac
-Cardiac
-Infracardiac
-Mixed
Supracardiac Type—Type I
- Most common (52%)
- Pulmonary veins drain into vertical vein (behind left pulmonary artery) to left brachiocephalic vein to SVC
l DDx: VSD with large thymus
Supracardiac Type 1—X-ray Findings
l Snowman heart = dilated SVC+ left vertical vein
l Shunt vasculature 2° increased return to right heart
l Enlargement of right heart 2° volume overload
Cardiac Type—Type II
l Second most common: 30%
l Drains into coronary sinus or RA
l Coronary sinus more common
l Increased pulmonary vasculature
l Overload of RV leads to CHF after birth
l 20% of I’s and II’s survive to adulthood
l Remainder expire in first year
Infracardiac Type—Type III
l Percent of total: 12%
l Long pulmonary veins course down along esophagus
l Empty into IVC or portal vein (more common)
l Vein constricted by diaphragm as it passes through esophageal hiatus
l Severe CHF (90%) 2° obstruction to venous return
l Cyanotic 2° right to left shunt through ASD
l Associated with asplenia (80%), or polysplenia
l Prognosis = death within a few days
Mixed Type—Type IV
l Percent of total: 6%
l Mixtures of types I – III
No comments:
Post a Comment